Critical Care Management (CCM)
Providing the Help that’s Needed for Your Members Who Are in Dire Straits, the 5% that Drive 60% of Your Health Plan Costs
Our programs utilize a highly-skilled, multi-disciplinary team whose sole focus is you and your least well members.
They may be receiving case management from your TPA or ASO, but still not getting the help they need. We believe you should have a service available that is focused on this special group of members in their hour of need, providing them with quality crisis care delivered cost effectively. EHG's Critical Care Management is a lot more than Case Management. It's Case Management + Second Opinions + Centers of Excellence + Legal Navigation and pressure. Case Management is only clinical, and it is often very limited, at that. Our Critical Care Management program is specifically for those valuable members who are suffering the most and who are the most costly. They are typically 5% of your members who are driving 60% of your healthcare costs.
"EHG's Critical Care Management is a lot more than Case Management. It's Case Management + Second Opinions + Centers of Excellence + Legal Navigation and Pressure. Case Management is only clinical."
Care team
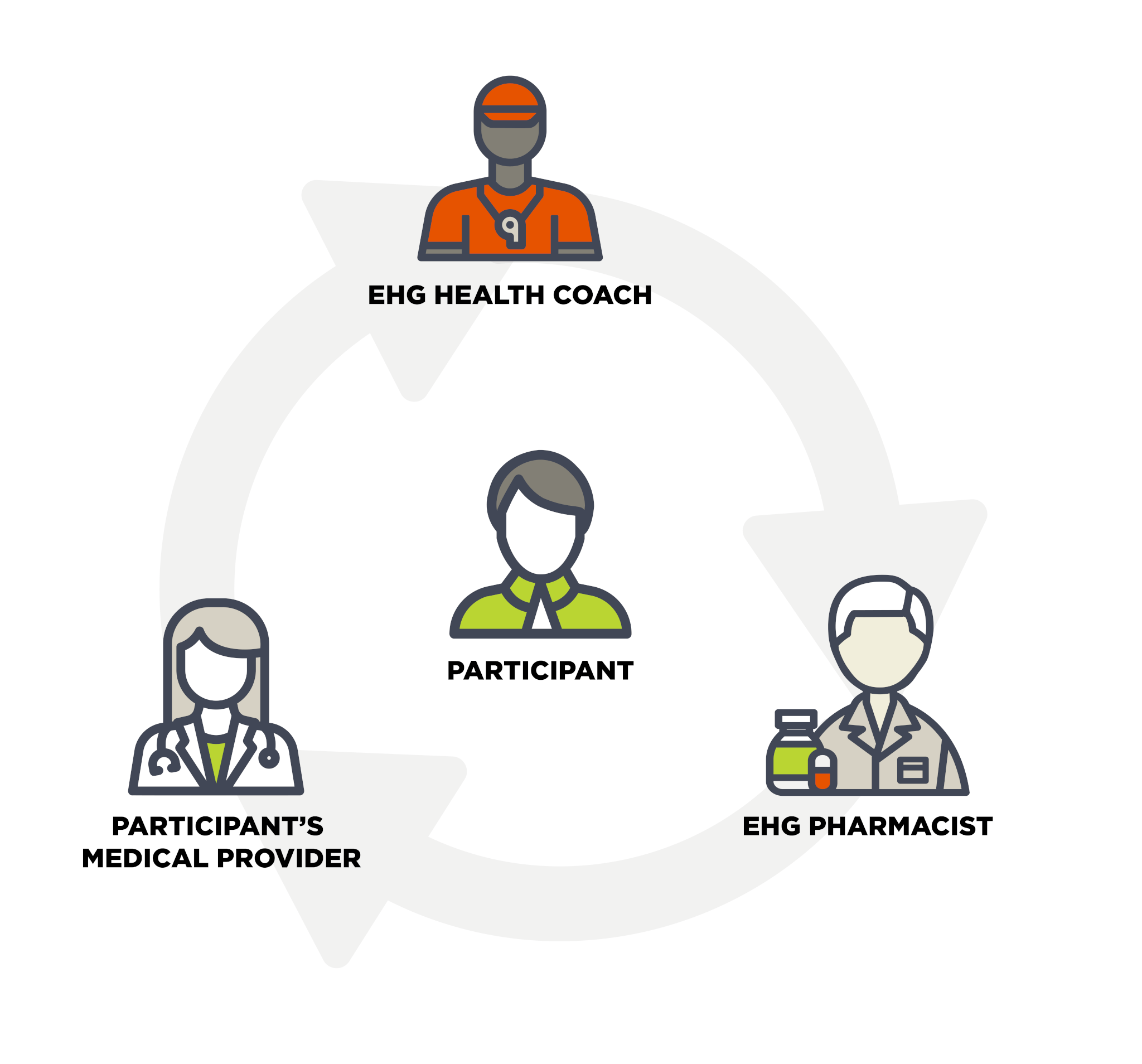
Our CCM program starts with relationships and engagement. At the foundation of our team is an EHG Behavioral Health Coach, who builds a relationship of trust and helps with accountability and troubleshooting. They are also assigned a medical Care Coordinator whose focus is getting the very best in specialty care. They are supported by an expert, multi-disciplinary team, consisting of physicians, physician assistants, nurse practitioners, and nurses.
Our team proactively engages with the highest risk members regularly, daily if needed, to design and deliver personalized care plans that include care coordination between providers & specialists, arrange second opinions and referrals to Centers of Excellence.
Our CCM team assures that the most traumatic, complex, and costly healthcare needs of your plan are being addressed at the highest level. We provide individualized coordination of care, record coordination, and a multiplicity of services 24x7x365.
Critical Care Management Team Toolbox:
Data driven
We leverage data from health screenings, healthcare claims, and other available health data and perform predictive health analytics to identify the members who are spending the most money on their care without getting the help they really need. The figure below shows the top ten conditions that we typically manage.
The member-level data that indicates treatments in process and gaps in care is based on health analytics, which can be provided to EHG by the client’s analytics partner or by the client’s benefits advisor. If neither of these sources can provide EHG access to the member-level data needed, EHG can also perform the analytics.
Since EHG collects health screening data, which is the best leading indicator of chronic disease, EHG can proactively identify and engage members who may not have been to the doctor nor filed any claims - but are at high risk for chronic disease. Therefore, our ability to engage 90% of the population in a health screening provides tremendous value into the ticking time bombs that are not showing up in claims yet.
The health screenings and analytics are essential tools to help avoid and/or minimize the impact of chronic disease. The high-risk members from our analysis and stratification are then assigned to an EHG health coach and the CCM team, who also keep each member’s Primary Care Providers engaged and informed.
Top ten conditions
- 1Cancer
- 2End-Stage Renal Disease
- 3Rheumatoid Arthritis
- 4Ulcerative Colitis
- 5Post-Covid Syndrome(s)
- 6Mental Health
- 7Premature Infants
- 8Fibromyalgia
- 9Post-Stroke
- 10Post-Myocardial Infarction Heart Failure
